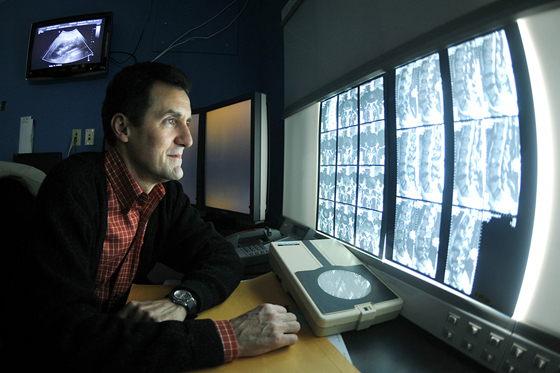
 As a Hodgkin’s lymphoma survivor, I’ve had plenty of CT scans, mammograms, chest X-rays and MRIs during my diagnosis, therapy and 20 years of follow-up care. So I’ve interacted with radiologists at many Bay Area clinics, including Stanford, where I was treated — that is, if you count getting summary reports in the mail as “interactions.”
As a Hodgkin’s lymphoma survivor, I’ve had plenty of CT scans, mammograms, chest X-rays and MRIs during my diagnosis, therapy and 20 years of follow-up care. So I’ve interacted with radiologists at many Bay Area clinics, including Stanford, where I was treated — that is, if you count getting summary reports in the mail as “interactions.”
This type of interaction may be changing with the growing movement toward patient-centered care, which is a critical component of the new American College of Radiology’s Imaging 3.0 initiative. Some radiologists are now going beyond image interpretation by discussing test results directly with their patients.
“Many interventional radiologists are now creating their own clinics, seeing patients and following them like any other surgeon,” Sandip Biswal, MD, a Stanford associate professor of radiology, told me. “Patient interactions are also quite heavy in mammography, particularly if the radiologist sees something suspicious.”
As radiologists come out of their reading rooms, many need to improve their communication skills, and a new training program at UMass Memorial Medical Center, called “Coming Out of the Dark,” teaches first and fourth-year radiology residents effective communication skills through role-playing. The program is led by Carolynn DeBenedectis, MD, an assistant professor of radiology there.
The participants practice six scenarios, such as delivering bad news from breast imaging tests, with trained actors performing as the patients. They are evaluated by both the patient actors and attending radiologists with prior communication skills training. The sessions are also videotaped and reviewed with the residents. The same participants return two weeks later to role-play six similar scenarios in order to evaluate their improvement.
At the Radiological Society of North America 2015 meeting, DeBenedectis reported on last year’s pilot program results. Participants were graded using a standard communications assessment scale and their scores on average improved about 5 percent between the two sessions — from 74 percent to 79 percent for first-year residents. More importantly, participants found the training useful, as reported in a recent online story.
We could probably all benefit from improved communication skills. However, there is some controversy over whether diagnostic radiologists should be communicating about imaging results directly with their patients after their scans. Biswal explained to me:
In the patient’s best interest, we really need to take a team approach. The primary care physician or referring specialist has the best understanding of what the patient is going through, so they can better convey the news. For radiologists to sit down with a patient and give them imaging results without knowing their full story can be potentially dangerous. There is an art to conveying this type of information that takes years of practice. I think of it like this: if it was my mother, how would I want her to be treated?
Jennifer Huber, PhD, is a science writer with extensive technical communications experience as an academic research scientist, freelance science journalist, and writing instructor.
Previously: Every foot has a story: Why communication is key in radiology, Education reduces anxiety about mammography and Study highlights need to raise awareness about radiologists’ role in health care
Photo by Offutt Air Force Base